India, as the world’s most populous country with over 1.42 billion people, faces an urgent need to manage its demographic trajectory. While population growth can fuel economic dynamism, it also intensifies challenges such as resource scarcity, healthcare burden, and social inequality. According to the United Nations, India’s population will likely peak around 2064 and gradually decline thereafter. The upcoming 2024 Census will play a pivotal role in validating these projections and shaping policy responses. As policymakers strive to address these challenges, reproductive health and contraceptive laws emerge as critical factors in managing population control and ensuring gender equity.
What Are Contraception and Termination of Pregnancy?
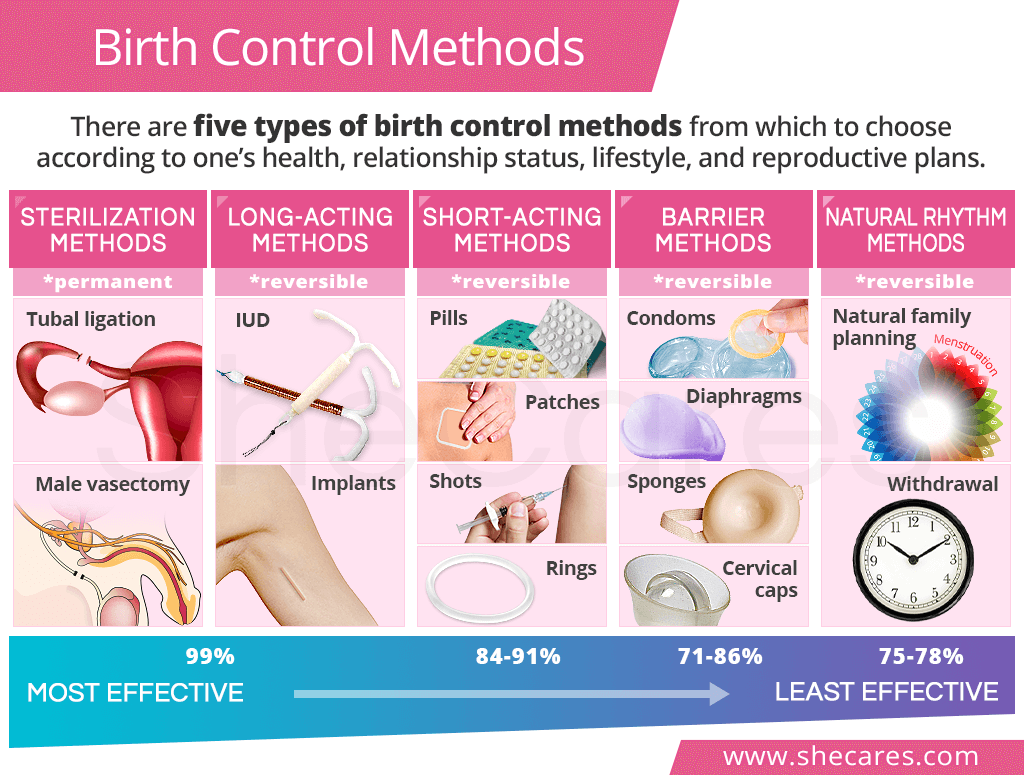
Contraception refers to methods used to prevent pregnancy, employing devices, medications, or surgical techniques. Examples include oral pills, condoms, and intrauterine devices (IUDs). Termination of pregnancy, or abortion, is a separate process that involves ending an established pregnancy either through medications or surgical intervention. The key distinction lies in timing: contraception prevents pregnancy from occurring, while abortion intervenes after conception.
Both processes have distinct legal and social dimensions. In India, the constitutional right to make reproductive choices, upheld under Article 21, affirms a woman’s right to privacy, dignity, and bodily integrity. This right was emphasized in landmark judgments like K.S. Puttaswamy v. Union of India and Suchita Srivastava v. Chandigarh Administration, which established that reproductive autonomy includes decisions to procreate or abstain from procreation.
How Are Contraceptive Services Regulated in India?
The Indian government, through the Ministry of Health and Family Welfare, implements contraceptive services under the National Family Planning Welfare Program. These services are widely accessible and often free, delivered through primary health centers (PHCs), sub-centers, and district hospitals. Accredited Social Health Activists (ASHAs) further ensure doorstep delivery of contraceptives, such as oral pills and condoms, at nominal charges.
India’s contraceptive options are categorized into spacing methods and permanent methods:
- Spacing Methods: These reversible methods allow individuals to plan pregnancies at their convenience.
- Oral Contraceptive Pills: Hormonal pills like MALA-N are distributed free under government programs.
- Condoms: Branded as Nirodh, condoms provide dual protection against pregnancies and sexually transmitted infections (STIs).
- Intrauterine Devices (IUDs): Long-term methods like Copper-Ts are highly effective for birth spacing.
- Permanent Methods: Irreversible options are often chosen by those who no longer wish to have children.
- Female Sterilization: Techniques such as minilaparotomy and laparoscopy involve blocking or cutting the fallopian tubes.
- Male Sterilization: Vasectomy, a simpler and safer procedure, involves blocking sperm-carrying tubes to prevent fertilization.
Why Is Male Participation in Sterilization Lagging Behind?
Despite being the first country to launch a national family planning program in 1952, India has seen a sharp decline in male sterilization rates. During 1966-70, 80.5% of sterilizations were vasectomies, but this number dwindled due to policy shifts and persistent gender biases. The National Family Health Survey (NFHS-5) indicates that male sterilization rates have stagnated at 0.3%, while female sterilization accounts for a staggering 37.9%. This gender disparity highlights the disproportionate burden on women.
The National Health Policy 2017 aimed to increase male sterilizations to 30%, but progress has been minimal. Factors contributing to the low uptake include:
- Cultural beliefs: Many men consider sterilization a threat to their masculinity or fear loss of libido.
- Economic constraints: Daily wage earners often avoid the procedure, fearing income loss during recovery.
- Lack of awareness: Many men are unaware of government incentives or the simplicity of the no-scalpel vasectomy procedure.
- Healthcare access: Rural areas face a shortage of trained professionals and inadequate dissemination of information.
What Can Be Done to Encourage Male Participation in Family Planning?
Several strategies can bridge the gap between male and female sterilization rates:
- Education and Awareness: Sensitization should begin during adolescence through school programs that emphasize shared responsibility in family planning. Awareness campaigns can dispel myths and normalize male sterilization.
- Cash Incentives: Offering financial compensation to offset income loss can motivate more men to opt for vasectomies. For instance, states like Madhya Pradesh have increased these incentives by 50%.
- Community Engagement: Trained health workers must actively educate rural populations about the benefits of vasectomy. Efforts like the “Vasectomy Fortnight” observed in India aim to debunk misconceptions and generate demand.
- International Models: Countries like South Korea, Bhutan, and Brazil offer valuable lessons. Progressive gender norms, media campaigns, and government-led camps have significantly boosted vasectomy rates in these nations.
How Do Gender Inequalities Impact Family Planning?
The disproportionate reliance on female sterilization perpetuates gender inequality. Women often bear the physical and emotional burden of sterilization, a practice that undermines their empowerment and contributes to health risks. Addressing these disparities is essential to achieving Sustainable Development Goal 5, which focuses on gender equality and empowering women and girls.
Field studies in rural India reveal entrenched attitudes that view sterilization as a woman’s duty. Many women expressed that men should not be “burdened” with the procedure, citing societal norms and economic hardships. Overcoming these biases requires sustained efforts to challenge patriarchal beliefs and promote equal responsibility in family planning.
What Are the Next Steps for India’s Reproductive Health Policies?
The path forward involves aligning policies with actionable goals to ensure reproductive health equity. Key recommendations include:
- Strengthening Healthcare Systems: Expanding training for healthcare providers, especially in rural areas, can improve access to vasectomy services. Investing in non-scalpel vasectomy techniques can make procedures safer and less invasive.
- Policy Revisions: Concrete steps, rather than intentions, are needed to bridge gender gaps in family planning. A demand- and service-focused approach can transform reproductive health outcomes.
- Cultural Shifts: Long-term social change is essential to normalize male participation in family planning. This requires consistent advocacy, community engagement, and mass media campaigns.
India stands at a crucial juncture where addressing population growth and reproductive health can pave the way for sustainable development. By promoting gender equality, improving healthcare access, and promoting informed choices, the nation can transform its demographic challenges into opportunities for inclusive growth.